Q.1. Which parts of the world the disease is prevalent?
Melioidosis is predominately a disease of tropical climates, prevalent especially in Southeast Asia and northern Australia.
Q.2. What is the causative agent?
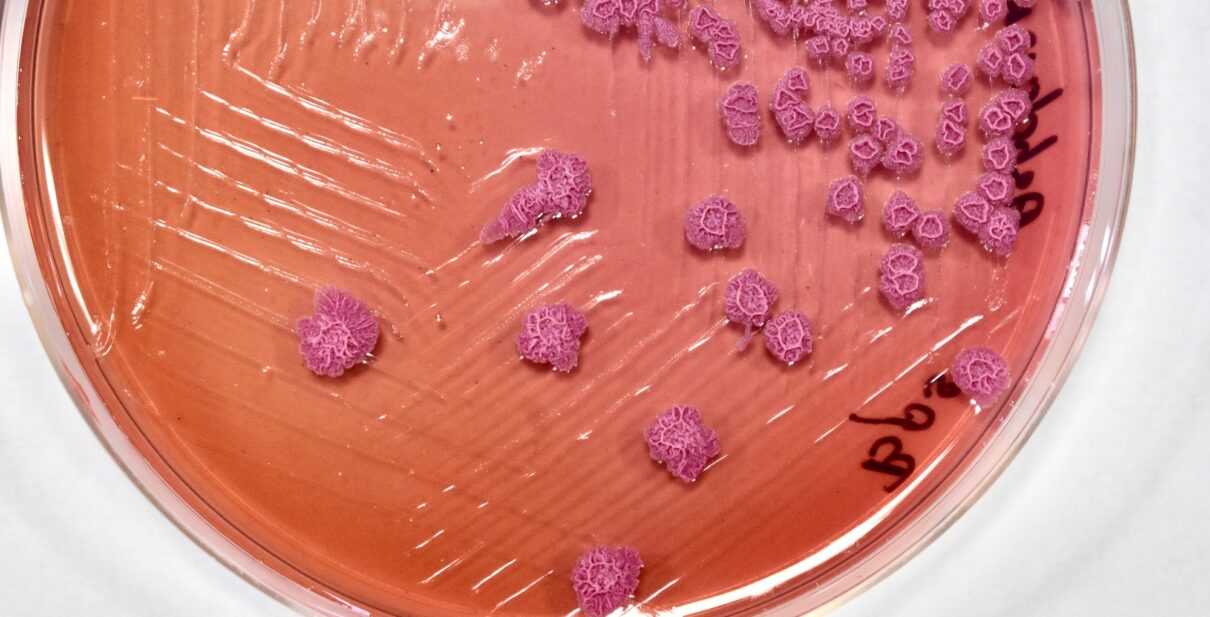
It is caused by the bacterial soil saprophyte B. pseudomallei, which is a tier 1 select agent for its biothreat potential.
Q.3. How does the bacterium invade inside human being?
This bacterium exhibits excellent genetic diversity and a capacity to evolve rapidly within the host. It is known to invade the epithelial cells of the mucosa or broken skin at its portal of entry and replicates within. Intracellular replication, survival, and spread occur in phagocytic and nonphagocytic cells. The organism can directly enter the bloodstream and infect antigen-presenting cells, causing bacteremia and sepsis. Additionally, entry into the lymphatic system contributes to the spread to secondary sites.
Q.4. What are the presenting symptoms?
The symptoms of melioidosis vary depending on the type of infection. These mostly include localized (symptoms include localized pain or swelling, fever, ulceration, abscess etc.), pulmonary (symptoms include cough, chest pain, high fever, headache, anorexia), bloodstream (fever, headache, respiratory distress, abdominal discomfort, joint pain, disorientation), and disseminated infections (symptoms include fever, weight loss, stomach or chest pain, headache, seizures). The significant risk factors for melioidosis include diabetes, liver disease, renal disease, thalassemia, cancer, and chronic lung disease (such as cystic fibrosis, chronic obstructive pulmonary disease and bronchiectasis).
Q.5. What are the probable sources of the bacterium?
Soil and water are the common habitats of B. pseudomallei. People who are in contact with soil and water and usually having the aforementioned comorbidities may acquire the disease.
Q.6. How does human being get the infection?
Humans and animals generally get the disease by inhalation of contaminated dust or water droplets, ingestion of contaminated water, and/or contact with contaminated soil, primarily through skin abrasions.
Q.7. What are the current challenges in diagnosing melioidosis cases in India?
• Lack of clinical awareness about the disease
• Lack of microbiological expertise to diagnose the disease
• Inadequate laboratory preparedness
• Lack of database in automated diagnostic system to diagnose B. pseudomallei
• Non-availability of automated blood culture system in may medical centers
• Hesitancy in reporting B. pseudomallei from the clinical samples
• Misleading or inadequate information in the text books used at the UG or PG level
• Lack of awareness about the disease at the national level while preparing any guidelines or policy
Q.8. Why melioidosis is an important disease in Indian perspective?
We estimate that a total of 939 melioidosis cases have been reported from 17 states of India from 1991 to 2021 within the age group of 0-84 years and with a mortality ranging from 8-50% (unpublished data from KMC, Manipal). According to a surveillance study conducted by the MoHFW, India, there were 1,88,401 cases of dengue detected in 2017, leading to 345 deaths (NVBDCP, DGHS, MoHFW, India). The report of IDSP (2019) documented that the presumptive cases of dengue are 44,069 whereas lab-confirmed cases are 18,145 (IDSP, NCDC, India, 2019. In leptospirosis, the presumptive case numbers reach 1033, whereas lab-confirmed cases are 568 (IDSP, NCDC, India, 2019). In contrast, we find that the estimated burden of melioidosis in India is 52,006 (22,335-1,24,652) cases accounting for 31,425 (13,405-75,601) deaths per year, which is much higher than the percentage of reports to death rate ratio each year than diseases like dengue, ebola, lassa fever, chikungunya and zika virus combined.